Basic Techniques and Surgical Pearls
Mastering Intracranial Microvascular Anastomoses
eBook with Online Videos
Basic Techniques and Surgical Pearls
Mastering Intracranial Microvascular Anastomoses
"The Lost Art of Microvascular Anastomoses...revisited!"
As you turn the leaves of this exquisite display of our specialty through simple, clear and pictorial instructions, aspiring surgeons or even masters of surgery, are able to acquaint themselves with not only the technical nuances, but also applied clinical pearls.
Garnette Sutherland (University of Calgary)
"An essential textbook on the techniques of cerebral revascularization surgery"
Kiyohiro Houkin (Hokkaido University Graduate School of Medicine)
"Pictures with detailed commentaries and our tips for surgeries are included."
Hiroyasu Kamiyama (Teishinkai Hospital)
Information
- Promotion video uploaded to Youtube
- Available at Amazon.com, iBooks.com, Kobo.com. Or check the above ebook stores of your country.
Foreword
- by Garnette Sutherland
-
The Lost Art of Microvascular Anastomoses...revisited!
In 1966, Yasargil and Donoghy performed a superficial temporal artery - middle cerebral artery bypass in a dog, followed by Yasargil conducting the procedure in a patient1). Following this, the neurosurgical community became active in refining surgical techniques for microvascular anastomoses, and translating these to the treatment of intra- and extra-cranial cerebrovascular disease, in particular occlusive vascular disease. The number of such procedures showed exponential growth. In this environment, due to uncertainty surrounding its beneficial effect in patients, a randomized controlled trial led by Henry Barnett was undertaken2). The trial results published in the New England Journal of Medicine on November 7, 1985, formed a seminal and historic awakening in neurosurgery, with a marked fall in the number of procedures performed. This was further substantiated by a second trial that stratified symptomatic patients with poor perfusion to EC-IC bypass or no bypass. Unfortunately the study was terminated due to futility, with only 2% chance for success from surgery if the trial was continued to completion3).
Surgeons continue to perform EC-IC bypass, for selected pathologies, in particular Moyamoya disease and to enhance cerebral blood flow in the indirect management of large-giant intracranial aneurysms. Unfortunately, even for aneurysms, with the introduction of endovascular techniques, EC-IC bypass continues a downhill spiral, towards almost becoming a dying skill... indeed many of the modern neurosurgeons and young graduates have never performed a bypass !
In the Yasargil era, young surgical trainees would rotate to laboratories to master the techniques of microvascular anastomoses. Serendipity or not, these surgeons realized a marked improvement in their overall surgical technique and finesse once back in the operating room. A short time away from patient, spent in the laboratory, enhanced and expedited the journey towards mastery in microsurgical technique. This introduced the art of paucity of undesired motion in the performance of surgery, and thus the philosophy of ideal force and tool motion.
In his “Mastering Intracranial Microvascular Anastomoses” manual, Dr. Taku Sugiyama, holds our hand and takes us back in time, to revisit this lost skill that everyone would crave. As you turn the leaves of this exquisite display of our specialty through simple, clear and pictorial instructions, aspiring surgeons or even masters of surgery, are able to acquaint themselves with not only the technical nuances, but also applied clinical pearls. While spending a short sabbatical in Calgary, Canada, this gifted and understated surgeon, was able to convince many young residents on the value of this proficiency. The excitement amongst this future generation of neurosurgeons was palpable, which led to Dr. Sugiyama, now sharing his teaching with the world. Enjoy the manual, and all the best on your journey.... towards mastery !
Garnette Sutherland
Professor of Neurosurgery,
Lead - Project neuroArm,
Department of Clinical Neurosciences and Hotchkiss Brain Institute,
University of Calgary1)Donaghy RMP, Yasargil MG (eds): Microvascular Surgery. Georg Thieme Verlag, Stuttgart, 1967
2)The EC/IC Bypass Study Group: Failure of extracranial-intracranial arterial bypass to reduce the risk of ischemic stroke. Results of an international randomized trial. N Engl J Med 313: 1191-200, 1985
3)Powers WJ, Clarke WR, Grubb RL Jr, et al: Extracranial-intracranial bypass surgery for stroke prevention in hemodynamic cerebral ischemia: the Carotid Occlusion Surgery Study randomized trial. JAMA 306: 1983-92, 2011
- by Kiyohiro Houkin
-
Cerebral revascularization surgery is becoming one of the most important and essential techniques in Neurosurgery. This technique is indispensable not only for cerebral ischemic disease but also for difficult aneurysms requiring surgeries.
I am confident that this book written by Dr. Taku Sugiyama is the best book on basic techniques not only for beginners but also experts of this type of surgery.The basic techniques introduced in this book were developed by Dr. Hiroyasu Kamiyama and our colleagues at the Department of Neurosurgery in Hokkaido University Graduate School of Medicine. These techniques are the crystallization of continuous efforts to develop and improve details of the techniques from all contributors. The Japanese version of cerebral revascularization surgery was published in 2000. We recognized the importance of translating this publication into English. However, we had been extremely occupied with routine work performing neurosurgeries and had been waiting for the appearance of new talent who could complete this mission.
Dr. Taku Sugiyama is an excellent neurosurgeon who has superb technique and experience in cerebral revascularization surgery. In addition, he has excellent skills in unifying these various techniques in a systematic way and publishing this information in English.
In addition, we were fortunate to have Prof. Garnette Sutherland on the team, who provided excellent suggestions and ideas to Dr. Sugiyama to complete this difficult task. Needless to say, this wonderful book would never have been published without the guidance and assistance of Prof. Sutherland.I am confident that this book will become an essential textbook on the techniques of cerebral revascularization surgery. I would like to express my sincere gratitude to MEDICUS SHUPPAN, Publishers in Osaka Japan who supported us throughout the process of completing this daunting task.
Kiyohiro Houkin
Professor and Chairperson Department of Neurosurgery,
Hokkaido University Graduate School of Medicine
- by Hiroyasu Kamiyama
-
When Dr. Sugiyama was training under my tutelage at our institute, he was still young and there were few opportunities for him to perform operations by himself. He mainly functioned as an assistant to other senior neurosurgeons, including myself. I appreciated his serious attitude with regards to training and this feeling of appreciation was also shared by other senior neurosurgeons. He subsequently continued further training, properly organized what he learned at our institute, and has now published this outline. The content of this current publication also includes information that I did not clarify, which shows Dr. Sugiyama’s outstanding insight.
At the time I entered the field neurosurgery, it was the introductory period for microsurgeries in Japan and both junior and senior neurosurgeons were obsessed with studying vascular anastomosis using rats. In those days, microsurgical training meant bypass surgery training using rats. I had a tendency to get immersed in what I was doing, wherein I tried to dissect and peel off the aortas and vena cavas of rats in order to study carotid artery anastomosis and arachnoid dissection every day until midnight (however, those procedures barely succeeded and most of the animals died due to blood loss!). After that, I was given an opportunity to become an apprentice with Dr. Zentaro Ito in Akita, who was a pioneer of Japanese microsurgery, and I was fortunately given a microsurgery training laboratory. We performed research on vascular anastomosis using YAG lasers. Dr. Ito had already been using high flow bypass procedures using radial artery grafts in clinical practice and he was the first to use these procedures clinically in the world. Furthermore, A3 - A3 side to side anastomosis, which we developed, has now become the standard procedure. Unfortunately, Dr. Ito passed away at the age of 44 in an accident, but his achievements were consolidated in a book called “MICROSURGERY FOR CEREBRAL ANEURYSMS (ELSEVIER / NISHMURA 1985).” This book includes Dr. Nobuyuki Yasui’s text and my illustrations. Due to our lack of experience, the book came short of what Dr. Ito aimed to achieve. However, at that time that was all we were able to do. Thereafter, the “Cerebral Revascularization Technique (2000),” “Cerebral Aneurysm Surgery (2010),” and other publications were published through the efforts of Dr. Houkin, an incumbent Professor at Hokkaido University. Subsequently, the “Introduction Guide: Clipping and Cerebral Revascularization” was published in 2014 as a predecessor of this book. This time, in order to address the shortcomings of the previous publication, pictures with detailed commentaries and our tips for surgeries are included. I believe this book will be extremely useful for neurosurgeons who are just starting to perform microsurgeries.
I also hope this book will be beneficial for all young neurosurgeons.
Hiroyasu Kamiyama
Brain Disease Institute, Teishinkai Hospital
March, 2017
Preface
- by Taku Sugiyama
-
This book introduces the basic technical nuances of microvascular anastomosis, as well as the fundamental concepts that lead to the success of intracranial bypass surgeries. Although bypass surgeries have been on a downward trend in recent years, these techniques are still necessary in some situations, such as for complex cerebral aneurysms, Moyamoya disease, and unexpected intraoperative vascular injuries. Bypass surgeries require both technical accuracy and proper understanding of the procedure. However, once these have been acquired, the success rate of bypass surgeries increases and consistent results can be achieved. Moreover, these techniques and knowledge would be beneficial in further advancing microsurgical techniques overall. Nevertheless, it is also true that younger physicians have limited chances to experience bypass surgeries. To help in this regard, this book was written with the aim of being easy to understand through the use of clear illustrations of surgical scenes. There is no greater happiness for me than if these techniques and knowledge could be spread through this book.
Most of the techniques and concepts described in this book were established through the initial efforts of Professor Hiroyasu Kamiyama and Professor Kiyohiro Houkin, and this wealth of knowledge and experience has been passed on to their apprentices and successors from generation to generation in Japan. Fortunately, I was able to organize and translate this information to English during my sabbatical at the University of Calgary from 2015 to 2017 under the supervision of Professor Garnette R. Sutherland. During this time, I was also able to obtain a great deal of invaluable knowledge and insights from him, including information not only on new surgical technologies but also novel viewpoints regarding microsurgeries. I would like to express my deepest gratitude to all of my mentors.
Since all of the surgeries in this book were performed at the Teine Keijinkai Hospital in Sapporo, I would like to express my appreciation to all the staff members at this hospital. It was the working experience at this hospital that made me grow the most as a neurosurgeon. I would also like to acknowledge Dr. Ken Kazumata and Dr. Naoki Nakayama for their continuous direct instructions on surgical techniques in the operating room.
This book could not have been published without the support of my unparalleled colleagues. Throughout the entire process of writing this book, Dr. Sanju Lama helped me in various situations. Dr. Michael B. Avery, Dr. Andrew Ryu, and Dr. David B. Israel provided constructive feedback and Christina Sutherland kindly helped me proofread the English translation. During the hands-on training courses held in Calgary, Liu Shi Gan, Fang Wei Yang, Kourosh Zareinia, Alison Shepherd and all the laboratory members of project neuroArm also provided tremendous support. My deepest gratitude goes to all the individuals who supported my efforts.
Last but not the least, my expression of gratitude would not be complete if I did not acknowledge my devoted wife, Saeko Sugiyama.
Taku Sugiyama
Department of Neurosurgery,
Hokkaido University Graduate School of Medicine
Project neuroArm,
Department of Clinical Neurosciences and Hotchkiss Brain Institute,
University of Calgary
March, 2017
Picking up suture with left-hand forceps for tying knot

Types of anastomosis
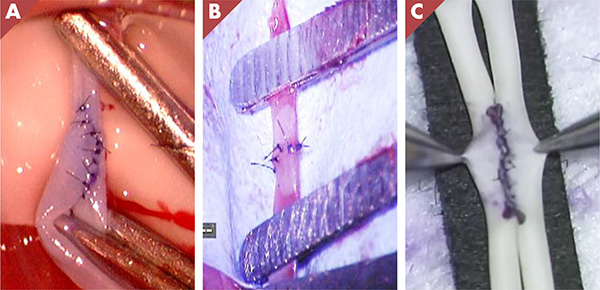
A: end-to-side, B: end-to-end, C: side-to-side
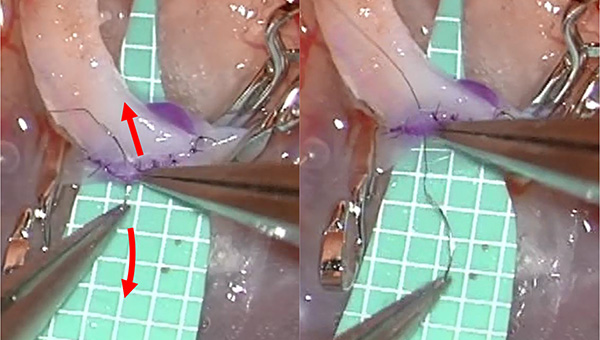
Extraction of the needle
Park-bench position and skin incision
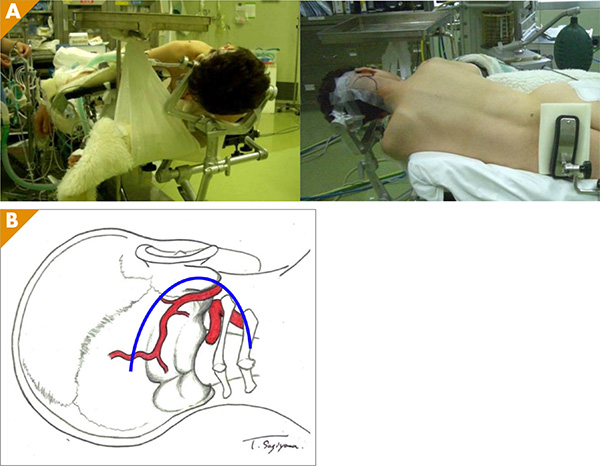
Table of Contents
Chapter 1 Suturing techniques
- 1: Surgeon posture
- 2: Holding jeweler’s forceps
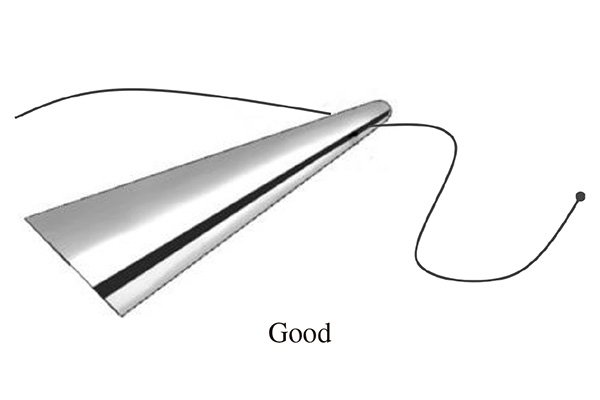
- 3: Positioning the needle
- 4: Passing the needle through tissue
- 5: Pulling the suture through, picking up the suture, and repositioning the needle
- 6: Tying knots
Chapter 2 Practical training
- 1: Materials used in bypass training
- 2: Instruments
- 3: Training methods
- 4: Chicken wing model
- 5: Rat common carotid artery model [Video1]
- 6: End-to-end anastomosis
- 7: Side-to-side anastomosis
Chapter 3 Technical nuances in microvascular anastomosis
clinical case
- 1: Preparing donor artery
- 2: Selection of recipient artery
- 3: Branches of the recipient artery
- 4: Setting of the surgical field
- 5: Design of the anastomosis
- 6: Preparation of the suture
- 7: Interrupted or running suture?
- 8: Clamping vessel
- 9: Arteriotomy
- 10: Ideal technique for passing the needle
- 11: Order of suturing
- 12: Insertion of the needle
- 13: Special techniques
- 14: Extraction of the needle and suture
- 15: Tying knots
- 16: Adjusting the microscope
Chapter 4 Superficial temporal artery to middle cerebral artery bypass
- 1: Setting-up and skin incision
- 2: Harvesting STA and craniotomy
- 3: Double bypass procedure
- 4: Single bypass procedure
- 5: Closure
- 6: Representative case -Complex MCA aneurysm [Video2]
- 7: Representative case -Progressive ischemic stroke
Chapter 5 Direct and indirect bypass for moyamoya disease
- 1: Direct and indirect bypass
- 2: Combined surgical procedure
- 3: Representative case [Video3]
Chapter 6 Special bypass procedures for revascularization of posterior circulation and anterior cerebral artery territory
- 1: OA-PICA bypass
- 2: STA-SCA and -PCA bypass
- 3: STA-ACA interposition graft bypass and A3-A3 anastomosis
Chapter 7 High-flow bypass for internal carotid artery reconstruction
- 1: Radial artery graft harvest
- 2: Positioning and opening
- 3: The route of the RA
- 4: RA-MCA anastomosis
- 5: ECA-RA anastomosis
- 6: Opening the RA graft
- 7: Surgical strategy using high flow bypass for complex ICA aneurysms
- 8: Representative case-An aneurysm in segment 1 [Video4]
- 9: Representative case-An aneurysm in segment 2
Video Table of Contents
- 2-5 Rat common carotid artery model [Video1]
- 4-6 Representative case -Complex MCA aneurysm [Video2]
- 5-3 Representative case [Video3]
- 7-8 Representative case-An aneurysm in segment 1 [Video4]